Female Genital Prolapse – Gynaecological Perspective
July 25, 2013 11:58 am
Definition
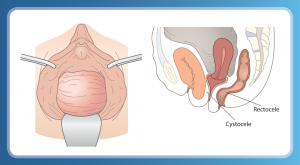
Prolapse/Procidentia is the downward descent of the uterus and/or vagina.
Procidentia is from the Latin, procidere, to fall.
It is not a disease but can be disabling for some women.
Effects of prolapse
The effects of prolapse range widely from no significant symptoms through
to local discomfort, loss of sexual function, urinary and bowel problems,
discharge, backache, ulceration and infection.
Causes of increased intra-abdominal pressure
There are six main causes (‘the six Fs’):
- fluid
- fibroids (and other tumours)
- flatus
- foetus
- faeces
- fat
When to treat
Treatment should be offered only when the condition is symptomatic and once it has been clearly ascertained that symptoms are due to prolapse.
Additional reasons for treatment may be that the condition interferes with a woman’s normal activity and that the patient actively seeks treatment.
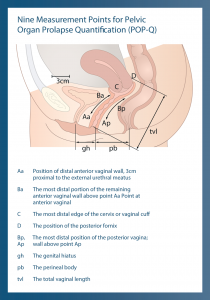
| Stage | Leading edge of Prolapse: Location of the Most Distal Point of the Anterior or Posterior Vaginal Wall (any points Aa, Ap, Ba, Bp) | Leading edge of Prolapse: Location of Apex of Vagina or Cervix (Value of Point C or D) |
|---|---|---|
| O | No prolapse: All points are 3 cm above the hyment (value = -3) | No prolapse: Apex of cervix is at a position above the hymen that equals or is less than +/- 2 cm of vaginal length (value |
| I | All points are more than 1 cm above hymen (value < -1) | |
| II | Maximal prolapse point protrudes to or beyond 1 cm above hymen but not more than 1 cm below hymen (value > -1 to > +1) | |
| III | Maximal prolapse point protrudes beyond 1 cm above hymen but less than 2cm less than the total vaginal length (value > +1 but < +(tvl - 2)) | |
| IV | Maximal prolapse point protrudes the length of the vagina (2 cm) beyond the hymen. Complete eversion of the vagina +/- cervix (value >/= +(tvl-2)) |
Treatment
- Pelvic fl oor exercises
- Prevent and limit injury during childbirth
- Topical Oestrogen Therapy
- Smoking cessation
- Avoid constipation
- Avoid heavy lifting
- Pessaries
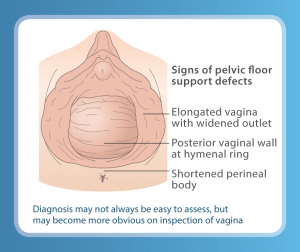
Diagnosis
- Examine patient
- Rule out pelvic pathology, e.g. pelvic mass
Pessary Treatment
Advantages of Pessaries
- Surgery contraindicated / declined
- Family not complete
- Temporary symptom control for those awaiting surgery
- May improve voiding dysfunction
Success Rate
Successful fitting rates are high varying from 74% to 94%. However in 46% of cases refitting within the first week may be required.
Problems
Poor fitting or the inability to retain a pessary may be influenced by the following:
- Deficient perineal body
- Large prolapse
- Wide introitus
- Vagina shorter than 6 cm
- Stenosed / atrophic vagina
A pessary could make stress incontinence worse or unmask stress incontinence.
The History of the Pessary
Used in the treatment of genital prolapse for centuries and is one of the oldest medical devices. It reached the peak of popularity in the 19th Century particulary to treat uterine retroversion.
Historical Perspective
Hippocrates mentioned the use of pomegranate to treat prolapse. The earliest written record on the use of pessaries is dated 27 BC and a papyrus from 1500 BC refers to prolapse.